Iron Deficiency in Women: Why It Is Common and How It Is Typically Addressed
Persistent fatigue, pale skin, or shortness of breath can sometimes be linked to low iron levels. Iron is a mineral the body uses to transport oxygen in the blood, and women are more likely than men to fall short of their needs at certain stages of life.
This article explains why iron deficiency is more common in women, which signs are often reported, and how diet and supplementation are typically approached in practice. The goal is to provide context and practical information, not to replace medical advice.
Why Iron Deficiency Is More Common in Women
Iron deficiency is one of the most frequently identified nutrient shortfalls worldwide. In women, several biological and lifestyle factors contribute to this higher prevalence.
- Regular blood loss during menstruation increases iron requirements.
- Pregnancy and breastfeeding significantly raise iron needs.
- Dietary intake may be lower, particularly in plant-based or low-meat diets.
These factors help explain why many women experience low iron stores at some point, even when overall calorie intake is adequate.
Commonly Reported Signs
Low iron levels can develop gradually. Symptoms vary between individuals and may be subtle at first.
- Ongoing fatigue or reduced stamina
- Pale skin or brittle nails
- Shortness of breath or faster heartbeat during effort
- Headaches, dizziness, or difficulty concentrating
- Cold hands and feet
Because these signs can overlap with other conditions, testing is usually needed to confirm iron status.
How Much Iron Do Women Typically Need?
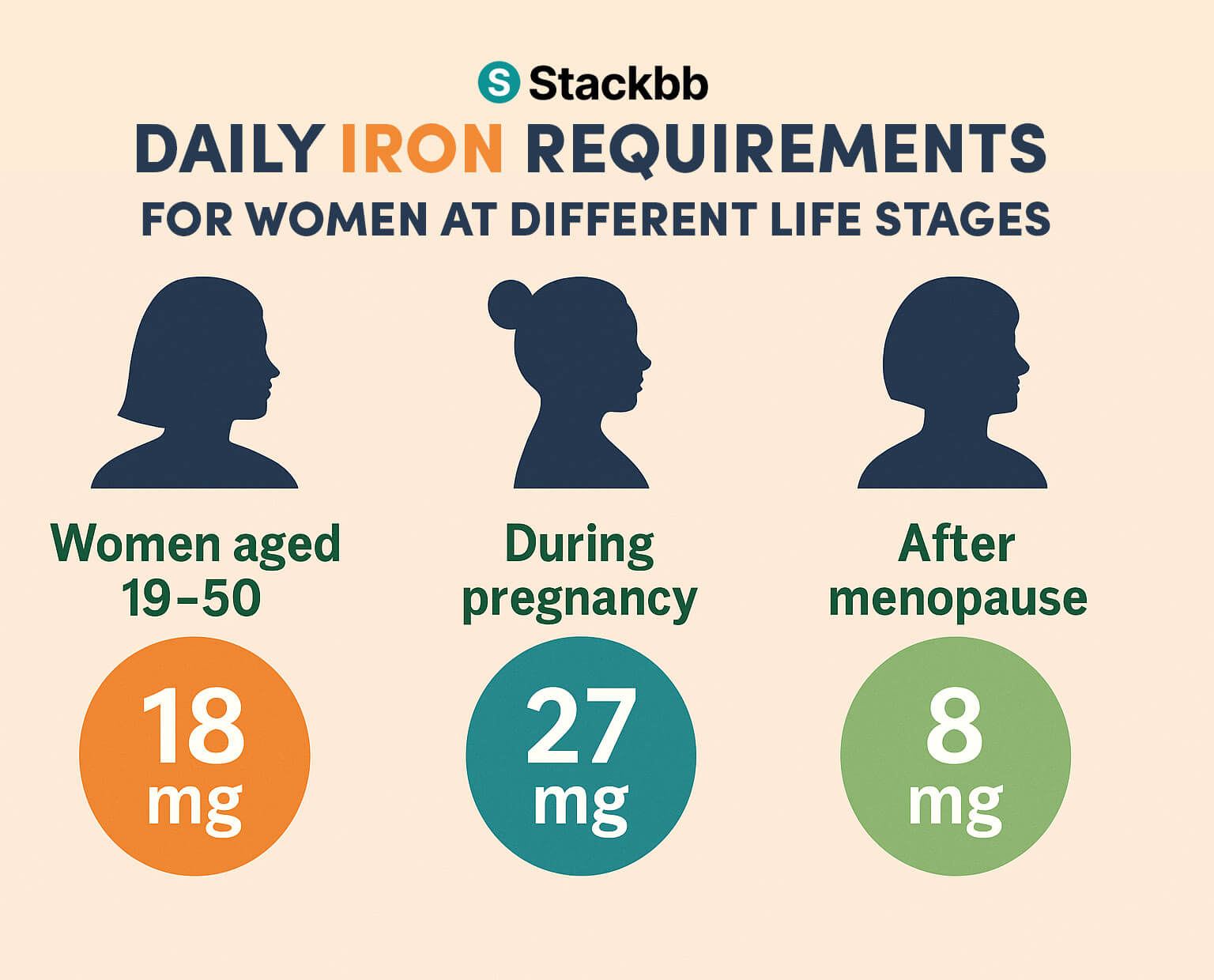
Source : https://medlineplus.gov/ency/article/002422.htm
Daily intake reference values
General intake recommendations vary by age and life stage:
Women aged 19 to 50 are usually advised to aim for around 18 mg of iron per day.
During pregnancy, this amount increases to approximately 27 mg per day.
After menopause, needs typically decrease to about 8 mg per day.
Dietary sources of iron
Iron from animal foods, known as heme iron, is generally absorbed more efficiently than non-heme iron found in plant foods such as beans, lentils, and leafy greens.
Combining non-heme iron sources with vitamin C rich foods, such as citrus fruits or bell peppers, can support absorption.
When Diet Alone May Not Be Enough
In some situations, meeting iron needs through food alone can be challenging. This is often the case during heavy menstrual periods, pregnancy, or when dietary intake is limited.
Supplement options that are commonly discussed include:
- Iron tablets or capsules: Available in several forms such as ferrous sulfate, gluconate, or fumarate.
- Liquid iron: Sometimes chosen by people who experience digestive discomfort with tablets.
- Multivitamins with iron: Usually contain lower amounts and are intended for general support.
The appropriate form and dose depend on individual needs and tolerance.
Digestive Tolerance and Side Effects
Some women report constipation, nausea, or stomach discomfort when taking iron supplements. Practical steps that are often suggested to improve tolerance include:
- Starting with a lower dose and increasing gradually
- Taking iron with meals, while avoiding tea, coffee, or dairy at the same time
- Trying a different formulation if symptoms persist
If side effects are significant or ongoing, professional guidance is recommended.
When Testing Is Commonly Considered
A blood test is typically used to assess iron status. This may be discussed with a healthcare professional if you:
- Have heavy or irregular menstrual cycles
- Are pregnant or planning pregnancy
- Follow a vegetarian or vegan diet
- Experience persistent fatigue without a clear explanation
Ferritin is often measured to evaluate iron stores rather than short-term intake.
Key Takeaways
Iron deficiency is common in women due to a combination of biological demands and dietary factors. Awareness of risk factors, attention to iron-rich foods, and appropriate supplementation when needed are typical parts of managing low iron levels.
If symptoms are present or risk factors apply, testing helps clarify whether iron intake should be adjusted.
FAQs
Why is iron deficiency more common in women?
Regular menstrual blood loss, pregnancy, breastfeeding, and dietary patterns all contribute to higher iron requirements in women.
What are early signs of low iron?
Fatigue, pale skin, brittle nails, headaches, dizziness, or shortness of breath are often reported, but confirmation requires blood testing.
How much iron do women usually need?
Needs vary by life stage. Women of reproductive age often require more iron than men, while requirements decrease after menopause.
Is food enough to maintain iron levels?
Many women meet their needs through diet, but some may require supplements depending on intake, absorption, and life stage.
Are iron supplements safe to use?
When taken at appropriate doses, iron supplements are generally well tolerated. Digestive side effects can occur and may require adjustments.
When is iron testing usually recommended?
Testing is commonly discussed for women with heavy periods, during pregnancy, with restrictive diets, or with unexplained fatigue.